by Beth Whitman
Mom stayed at home with Dad and me until she was physically unable to stand. The other determining factor in her decline from Alzheimer’s was that she had become overwhelmed with free-floating anxiety, irritability and fear that had been steadily increasing for about six months.
Her level of distress had started to get out of control, and regular anxiety medications, like Lorazepam, had ceased to be effective. But we had found a dosage of the anti-psychotic Haldol that seemed to keep her relaxed and alert and happy, or at least as happy as any normal person could possibly be when they are faced with no longer being able to function as they used to.
Nevertheless, it soon became impossible to care for Mom at home, and Mom knew it. So we initiated the process of moving her to an Alzheimer’s care facility.
The day of the move she was alert and engaged, and when we got to the facility she was delighted to see new faces and be around the hustle and bustle of activity. There was a noticeably positive bounce in her overall condition. She was again reading short sentences aloud and answering questions with relative coherence. When the doctor came to examine her, he was impressed with her functionality. So impressed, in fact, that he recommended taking her off all medications.
When I heard that I was shocked. We had worked hard to keep Mom functioning with a minimum of medications but now, based on the briefest of encounters, the doctor was going to take an action that I was certain would cause a lot of stress for Mom.
I spoke with the doctor, saying that I completely disagreed with him and that I did NOT think Mom should go off the medications. I said that I understood his impulse, and that I agreed in principle that reducing and even removing medication was a good idea. Indeed, as Mom’s primary caretaker for the past two years, I did not give her medications lightly. I had only used them as a last resort, and that was because Mom needed it. I told the doctor in no uncertain terms that, if she were taken off the meds, within three days she would become inconsolably agitated.
The doctor overruled me. He took her off all medications.
And sure enough, three days later, I came in to visit Mom, and as soon as I walked through the main doorway, I heard a high pitched “WO WO WO WO WO WO WO… NO NO NO NO NO NO NO” coming from down the hallway. Mom was clearly in a disturbed state. When she saw me, she stopped briefly, reached out to me and stuttered, “I, I, love you,” but within a minute, the keening started again, increasing in pitch and volume. “BU B B BU B BU B B B,” she sang out like an opera singer in pain. The staff was at a complete loss — they didn’t know what to do.
I asked if there was a pill they could give her. But the doctor had left no orders, so I went out to the car and got some of the pills that were left over from her prescription. I gave her one and stayed with her, holding her hand and walking with her up and down the hallway until she calmed down a bit. I came in as many times as I could that weekend, to slip her pills, but I was not able to make it in on a regular basis, and her level of distress, though somewhat reduced, was still high.
When the doctor came in on Monday morning, the staff brought him in to see Mom. She was still ululating. He took one look at her and immediately reinstated her prescription: 1 mg Haldol, 3x per day.
This stabilized her, but a month later he wanted to cut her dosage in half. Against my wishes once again. He insisted, and I went along with it as long as she could have access to additional doses “as needed.” I was coming in at least every other day, so I was able to keep a close eye on her and she seemed fairly stable.
A couple of months after that, the doctor said he was concerned with muscle rigidity and wanted to reduce her medication by half again. Muscle rigidity is an irreversible side effect of Haldol, so I understood the doctor’s concern, but I had not seen any evidence of muscle rigidity myself and, besides, I felt that “permanent” was a relative term in someone with late-stage Alzheimer’s. The potential for muscle rigidity needed to be seriously weighed against the already established benefit of effectively keeping agitation and distress at bay.
I was also a little mystified by the thought that someone was seeing muscle rigidity when I was not. So I asked Mom’s hospice nurse (not a regular employee of the facility) to show me what that rigidity would look like. We held Mom’s hand and did the test for rigidity, but it wasn’t there. I started to wonder if Mom was perhaps tensing up around the doctor because she generally resisted being examined. (Her entire life she had resisted seeing the doctor, and the resistance had just gotten more intense as her Alzheimer’s disease progressed.)
Shortly after the second reduction of Haldol, Mom began to show signs of being on the edge. She was not constantly ululating like she had been before, after the doctor took her off the meds completely, but there was a constant distraught expression on her face, and it didn’t take much for her to go back into her plaintive soprano song of “wo wo wo wo wo WO WO WO WO WO…”
Although “as-needed” pills were prescribed in addition to the regular dose of Haldol, I sensed a resistance among the staff to actually dispense an as-needed pill until she was well into an episode. I would often walk in and she would be in distress; however, it was not until I requested the additional medication that they would provide it. I began to automatically order an “as-needed” dose if I saw any sign of distress whatsoever.
I again enlisted the hospice nurse to help me convince the appropriate people at the facility to bring Mom’s dose back up to a level where she was no longer on edge. But I remain unnerved by how much of a battle it has been to keep Mom on a level of medication where she was not consistently agitated.
I know that Alzheimer’s facilities have faced complaints in the past that they over-medicate patients in their care, and I was wary of this potential from the start. But I was unprepared for the fact that the pendulum has swung the other way. Now, as a consequence of the previous reputation, the trend in Alzheimer’s facilities is to under-medicate their patients.
The other thing I was unprepared for was the difference in the cost of the medications themselves.
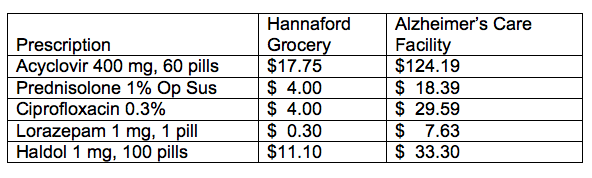
Because Mom was so healthy prior to her Alzheimer’s, she had chosen to forgo her Medicare Part D Prescription Insurance. So we had been getting her prescriptions filled at our local Hannaford (Maine) Grocery Store. The monthly costs were reasonable, but when Mom entered the Alzheimer’s care facility, we were no longer able to get the prescriptions filled there. Though the Patients’ Bill of Rights allows the residents of the facility to choose where they purchase medications, there is a requirement that all medications come bubble-wrapped, and Hannaford does not bubble-wrap. Instead, we had to go through their designated pharmacy where the costs for the same meds were shockingly higher.
To get a sense of how much higher, take a look at the following comparison:
I considered fighting the stipulation about bubble-wrapping, given that it has increased the cost of Mom’s prescriptions by more than 1000% in some cases, but I’ve grown weary of fighting battles on every front. I’m trying now to be selective about the battles I fight, so that I can focus my energies for the challenge of Mom’s declining condition.
I have to say, the most difficult thing about caring for Mom has been the almost constant energy and attention that’s needed to surmount all the various administrative issues, such as insurance problems, reimbursements, indecipherable bills, monitoring the in-home-care help, figuring out how to access and pay for the nursing home, or hospice (which was a little easier) — it’s an endless bureaucratic obstacle course. Or having to make an emergency visit to the Social Security office when, for some unknown reason, Mom’s payments suddenly stopped arriving.
With every turn, every new little glitch, I had to go through a laborious process of re-establishing myself as someone who could speak for my mother. Even with a full legal and medical Power of Attorney, I still had to go through the process of transmitting and re-transmitting that information to each organization, sometimes having to fax a single place four or five times a day just to get it through, and then calling back every few days to see if it had arrived yet. Sometimes the various systems seemed positively byzantine. The worst was Social Security, which, unlike the rest of the civilized world, doesn’t recognize a Power of Attorney. They have their own designation, called a Representative Payee. In order to attain that designation, one needs to provide two items: a letter from your parent or loved one’s doctor saying that the parent or loved one is too incompetent to represent themselves, and a letter signed by the parent or loved one — you know, the “incompetent” one — designating you as their representative.
It’s the Catchiest-22 of all Catch-22s.
Beth Whitman lives in Maine and is a member of Belfast Cohousing and Ecovillage, a developing community on the coast of Maine focused on multigenerational living and sustainability.







Beth, We are at the beginning stages of this with my mother. I have POA, and we live in FL. I was unaware of this Social Security issue. Is that in every state? What else do I need to do. Mother is still cognitive, but not always agreeable, so she may not understand why she needs to sign another form.
As the DON at a nursing home, I feel your pain! The rules are so unfair about the antipsychotic drug use and requirement to reduce the dosages. I’m sure that there are those facilities that “drug” their residents inorder to restrain them chemically, but mine is not one of those. I just need my residents to receive the drugs required to assist them to LIVE without unnecessary stress. It is so sad to watch the residents and their families suffer because of the unexpected and unusual behaviors! The rules are made by folks sitting behind desks in our political system that haven’t probably ever been in a NH for more than a few minutes!
Karen, You should talk to the Social Security office. I think the chances are that there wouldn’t be a real NEED to have yourself as Representative Payee, but if there are any issues that come up (such as when the payments suddenly stopped coming for my mom), Social Security will not even talk to you or try to resolve the issue without you being the Representative Payee OR by talking directly to your mom and having her answer a series of questions that confirm to them that she is who she/you say she is.
When this happened to us, mom was still cognizant enough to answer questions like “what is your name”, and could read a series of numbers and words (our phone number and address) if I wrote it down and put it in front of her and prompted (quietly) her to read it in response to the question posed to her on the phone. But she needs to be able to answer THREE questions correctly. I had to call back five times until I got someone at the Social Security office that was sympathetic and would work with us (because if they get any sense that the person is being prompted they will deny you). The sympathetic woman that we finally got on the phone went through a series of question that mom could not answer and finally hit on “what is your father’s name?” I ran and got a picture of mom’s father that was sitting on the shelf, and mom took a look at it, and said “oh, that’s daddy!” Then I turned the picture over and it had his full name written on the back. She read the name aloud, and the two of us (me and the Social Security woman on the phone) breathed a sigh of relief.
THEN, and only then, would they even confirm whether the payments had been sent or not.
My father suffered from Alzheimer’s and I understand your frustration. The signs your mother is experiencing are common but believe me the concern about over medicating is a real concern. Haldol is usually very detrimental to ALZ’s patients . Some hospitals use it not to be bothered with more humane patient care. My father’s neurologist did not approve of it and we could see the horrible results and he recommended not taking him back to that hospital. A good facility would have music therapy and other types of methods that seem to calm many patients. BEth,If your mother can still read she is not in an advanced stage. There is lot of misinformation and many other types of Dementia are incorrectly labeled ALZ. Rigidity is very common in other types of dementia such as Lewi body or Frontal Lobe dementia. My father was walking and pacing almost all night, calling out for his brothers so we would lock arms with him and try to speak in a soothing tone . We tried aromatherapy and Lavender seemed to help a bit as it did Valeria capsules. Just enough to give him a bit of rest. Music and singing to him his favorite hymns helped.
We were able to keep my dad home until the end. He died of a massive stroke when he was in the next to last stage. It took 4 family members determined to keep him in the place he knew best and where loving, though tired wife and daughters took care of him. There was no fortune and finances were tight. His insurance did not cover the ALZ medication back then.
I continue to receive training and being an advocate. I also recommend enrolling your loved one in a Memory Disorder study that most big hospitals offer. They will do a brain biopsy post- mortum and send you a report to confirm if it is was really ALZ. It will not help your loved one but it is helping in research and it could benefit you in the future.
Rosario, I understand your pain. Your father passed away before he reached the last stage of Alzheimer’s so perhaps it is very hard for you to understand what it is like to care for someone in the last stage of Alzheimer’s.
You are right, when a person is walking and reading they are not in an advanced stage of Alzheimers, and I am glad you are able to recognize that. However, when a person can no longer read or walk they ARE in an advanced stage of Alzheimers, and I hope you are also able to recognize that as well. I know it is difficult for you, but have patience, and God bless you.