by Kim Keller
The decisions we made still haunt me. And I suppose they always will.
It’s not that I think we made the wrong choices. In fact, I’m certain we made the right ones. What I can’t shake is the belief that my father should have been leading the discussion about his own healthcare choices.
Instead, he wasn’t even a participant.
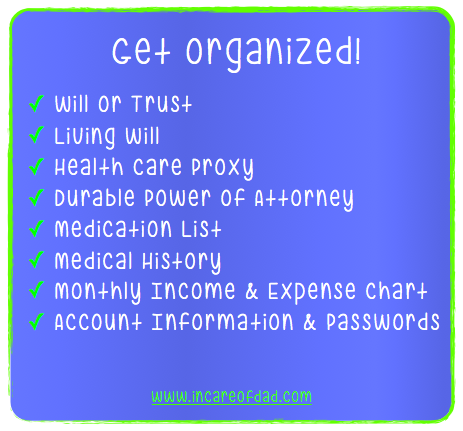
My dad had a living will. So my parents thought they were covered when it came to the recommendation, “Have a discussion with your family about end-of-life issues.”
But missing from that recommendation was the word “thorough” — as in, “have a thorough discussion about end-of-life issues.”
The living will only told us that Dad didn’t want to be kept alive by artificial means. What the document never anticipated were all of the other more likely scenarios that could develop. When some of those unforeseen events did ultimately play out, it was too late to secure his input and guidance.
Making these critical decisions for someone we loved so much, such as stopping aggressive medical treatments or starting hospice care, was a major impetus in the creation of In Care of Dad. My sister Karen and I wanted to spread the word: Have those end-of-life discussions before it’s too late, and make them meaningful!
Which often prompts people to ask us, “So how do I do that?”
Continue Reading