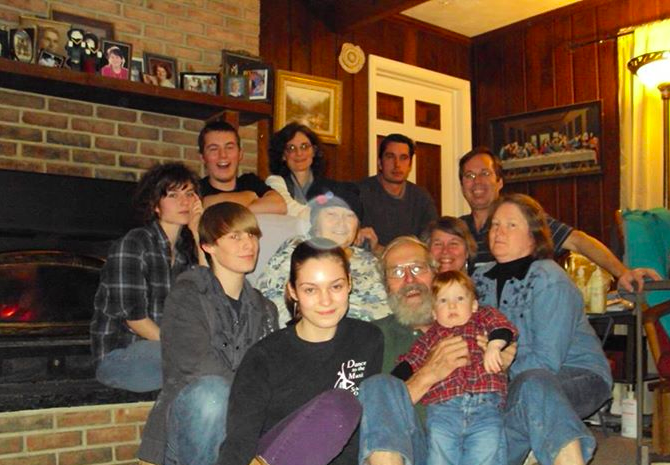
Cynthia’s dad in 2010.
We are pleased to share this blog with you. It first appeared on Cynthia’s WordPress site in April 2015.
by Cynthia Greb
What do you call a birthday when that person is no longer on this earth? I guess it’s still the anniversary of his birth, although we are no longer counting the years he has lived.
Dad’s birthday is April 30th. I wrote the first draft of this piece back in February on the first anniversary of his death. But then I set it aside to read it and revise it later. And “later” turned into another month. And now I’m dusting it off one more time.
It’s not easy to remember death.
There are so many wonderful, wonderful things to remember about Dad: his teasing and horsing around; his affection for his wife, kids, and especially his grandchildren; all his years of hard work supporting his family and never complaining; his love of naps; the way he always had time for his family; his dedication to the churches he attended and served; all the little vacations we took together; his love of food; his gregarious personality; his gratitude; his love of nature. I could go on and on. But sadly, I seem to be stuck in an endless review of his last few months.
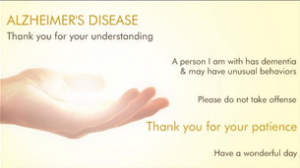
If he had started to drastically decline and then simply continued that decline, I think I could have accepted that. After all, death comes to each one of us, and after several years suffering the indignities of Alzheimer’s, I’m sure, at some level, he was more than ready to let go of this life. As a matter of fact, for several months, while he was still living in his home, he would repeatedly tell us, “I’m ready to go home. Please take me home. Please take me home.”
We had thought he was confused and couldn’t remember that this was his own home. We tried in vain to convince him that this was the home he’d built with his own two hands when the rancher had become too small for his burgeoning family. We pointed to all the pictures of the family on the mantle. We said, “See? There we all are! This is your home.” But it made no difference. He was caught in a sad loop, not realizing he was in his own home.
At least that’s what we thought at the time.
Continue Reading