by Kim Keller
Stress and anxiety chip away at our ability to concentrate. Left unchecked, we can become paralyzed, virtually unable to move forward effectively in our lives.
Here are 20 simple actions you can take to reduce stress and regain your mental focus:
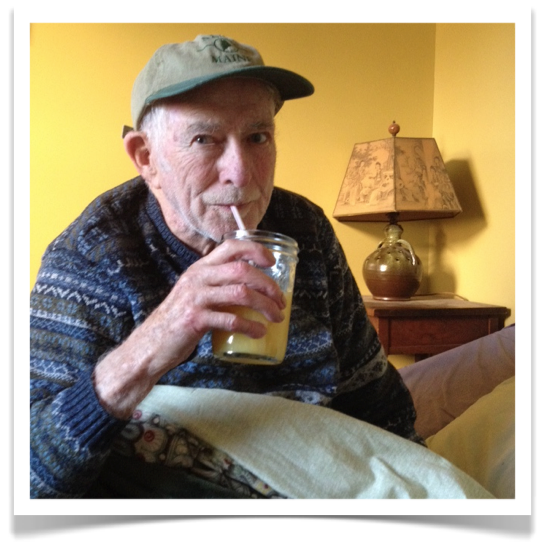
- Stay Hydrated — Water transports oxygen throughout your body, which in turn boosts your energy level and helps keep you alert.
- Wiggle Your Toes — Sounds silly, I know, but this great little “mindfulness” trick brings you back to the present moment and helps you refocus. Olivia Fox Cabane recommends this tip in her book, The Charisma Myth. Try it sometime.
- Create a Routine — Having a regular daily schedule simplifies life, which consequently eases stress by removing a major issue (laying out your itinerary for the day) that used to occupy your brain.
- Use the Mind Dump Exercise — When my brain is flooded, this exercise gives me comfort: I take 10 or 15 minutes to write down, as fast as I can, anything — anything at all — that comes to mind. It often starts with something like this: Why am I feeling SO stressed out?! I need to stop saying yes to everything! I need to get more sleep. All I want to eat is junk food! And on it goes. While the pages I create tend to be jumbled and chaotic, the exercise helps relieve anxiety and produce a sense of mental clarity.
- Don’t Worry Alone — Ned Hallowell, M.D., a bestselling author and world-renowned expert on ADHD, offers these next four tips, starting with Don’t worry alone. “Worrying alone tends to become toxic,” writes Hallowell, “because in isolation we lose perspective.” The benefit of sharing your fears and concerns is that “when you worry with someone else, you usually end up problem solving, as you feel more empowered and less alone.” So find someone to talk with and get the worries out of your own head.
- Get the Facts — “Toxic worry is rooted in wrong information, lack of information, or both,” explains Hallowell. Spend the time you’d normally waste on worry by getting the facts and learning what is true.
- Make a Plan — Use your energy to create a plan that helps you work through the problem, instead of using your energy to worry and fret. A plan will make you feel more confident and in control of your life.
- Think Happy Thoughts — “Thinking of things that promote warmth, connection, and happiness reduces the hormones associated with stress, fear, and anger that can impede concentration,” says Dr. Hallowell.
- Create a To-Do List — Trying to remember all of the little tasks on your plate takes too much mental effort. Instead, keep a list of everything you need to do, no matter how big or small, all in one place. I find it useful to review the list each night and make a smaller list that separates the items based on the tasks that must be completed the following day and those that I’d like to complete but aren’t quite as urgent. A to-do list is a great way to reduce anxiety.
- Use All of Your Senses — Make a point of practicing mindfulness by engaging all your senses. Next time you look at a tomato, for example, smell it, touch the skin, appreciate the shade of red, and, of course, taste it. Apply your senses whenever you can, and not just the most obvious ones. Take a moment to listen to the sounds of the day. Touch and smell things you normally just look at. Bring your entire sensory arsenal to bear on your everyday encounters.
- Noise-Canceling Headphone — To protect myself from distractions, I take breaks from phones, email, texting, etc., by wearing noise-canceling headphones and listening to music without words. This amplifies my focus and helps me fixate on whatever I’m trying to accomplish.
- Schedule Time to Worry — To avoid continual, uncontrolled worry, I find it helpful to allow myself actual worry time: I’m not going to worry about this tonight, I’m going to sleep, and I’ll make time in the morning to stress about this. It only works, though, if I make a pact with myself to devote equal time to reflect on what’s good in my life. This combination of scheduling worry time and giving equal attention to gratitude never fails to give me perspective. And comfort.
- Work in Small Doses — Whenever I’m overwhelmed, yet eager to be productive, I set a timer for, say, 10 minutes and then force myself to concentrate fully throughout the short time frame. When the timer goes off, I take a quick break, then I start again. At the 45-minute point, I take a longer break — 15 or 20 minutes. I’ve used this timer technique for years, and I just recently found out that there is an actual name for this approach: it’s called the Pomodoro Technique.
- Know Thyself — We all have times during the day when we can best focus; mine is in the morning. I try to organize my day so that anything requiring a lot of concentration and brainpower happens in the morning.
- Move — Take a walk, dance, run up and down the stairs, anything to wake up your body and your brain.
- Get Rest — The converse to number 15 is also true. Sleep is a great healer. For the longest time I just accepted the notion that I wasn’t a good sleeper, that I wasn’t blessed with that particular gift. But in recent years I’ve come to realize that my inability to sleep well was just another bad habit I needed to break. So I’ve put a lot of thought and effort into the subject, and that prompted a number of In Care of Dad articles. These, in particular, I found helpful. Take a look. Sleep Strategies Part One and Part Two.
- Clean a Closet — Removing clutter and getting organized gives you a sense of accomplishment and a great lift. It creates momentum to tackle even larger problems.
- Memorize Something — Memorization keeps your mind sharp. Try a poem or the US state capitals. If that gets too easy, learn the lines to your favorite play.
- Eat Well — Reduce your sugar and caffeine intake. Eat foods that will give you natural energy, like fruits and veggies. Create a diet for yourself that reflects excellent nutritional balance.
- Take Time to Meditate — I know, I know, when you’re stressed out and overwhelmed, who has time to meditate? But trust me, finding 10 minutes a day to focus on your breathing and your inner calm will set the tone for you. Just get started. First thing in the morning, before your coffee, set your timer for 10 minutes, find a quiet spot to sit comfortably, close your eyes, and take in a deep long breath. Hold it for a moment and then release a long slow exhale. To get me in the proper frame of mind, I say “in” as I take that deep breath, and then I say “out” as I let go and exhale.