by Joan Blumenfeld, MS, LPC
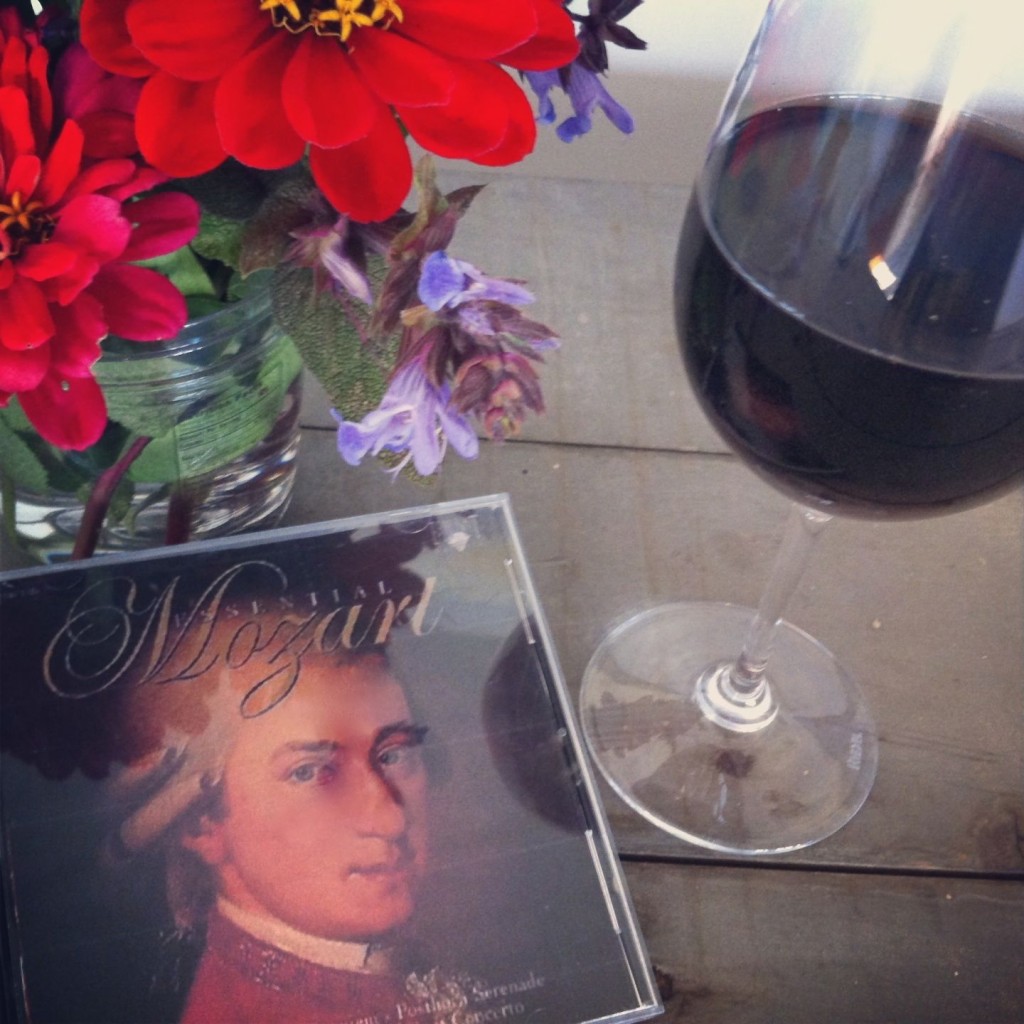
If I’ve told my children once, I’ve told them a thousand times. “When I’m near the end of my life, give me a good glass of wine, play me some Mozart, and LEAVE ME ALONE!”
I’m being only partly facetious. The wine and the Mozart are easy. Leaving me alone without trying to fix me is the wrenching part. Believe me, I know. I muddled through this process with three family members whom I loved deeply, and I’ve watched families of my frail, elderly clients go through the same experience.
Even when advance directives and living wills are as specific as they can be regarding Do Not Resuscitate orders, feeding tubes and ventilators, families still struggle with the decisions. There are conflicting views within the family, as well as conflicting medical advice, not to mention the uncertainty and fear in their own hearts and minds.
I have seen it happen repeatedly in my practice as a geriatric care manager. Mom or Dad sign a living will requesting that they not be resuscitated, tube-fed or ventilated. They want to be kept pain free and comfortable when they are nearing the end of their lives. They do not want interventions that prolong their dying but do not improve the quality of their lives. Yet their adult children find it impossible to adhere to those requests. It is too hard to let go. Focusing on comfort care, rather than fixing and curing, frankly feels too much like euthanasia.
Medical professionals often have the same difficulty letting go and are sometimes not very supportive of families who favor hospice and palliative care for their loved ones. It goes against the grain of their medical training.
So perhaps we should consider what quality of life means and whether quality of life or quantity of life is the ultimate goal of the elder. Some factors that constitute quality of life and make life worth living for me are:
- Being physically comfortable, pain free and secure (able to close my eyes and not be afraid).
- Being able to sustain important relationships.
- Having the ability to communicate.
- Being able to experience enjoyment and pleasure.
- Being able to engage in meaningful activity.
- Retaining some functional capacity.
- Living with dignity and individuality and NOT being a burden on my family.
When these qualities of my life are overwhelmingly and consistently compromised, with little realistic hope of recovery, then I want my children to bring in hospice, focus on comfort care and let me die a natural death with dignity.
Pearl of wisdom: Talk with your parents about their end-of-life wishes. Do it early and often. Encourage them to put their wishes in writing with the help of an elder law attorney. Read the superb booklet, Hard Choices for Loving People, by Chaplain Hank Dunn, which can be obtained at www.hardchoices.com.
Joan Blumenfeld, MS, LPC is a Geriatric Care Manager in private practice in Fairfield County, CT. For information, visit www.joanblumenfeld.com. © Joan Blumenfeld, 2013.






Just to throw out an argument that would answer some ethical questions regarding hospice – why in the light of hospice would euthanasia be so bad. I am always curious as to why hospice would be preferable to euthanasia. It concerns me that if the patients comfort is so impacted without help of chemicals why is euthanasia not a more comfortable & shorter term option & why as family and society are we so willing to embrace the morphine but not let them go painlessly & quickly. In the case of hospice and how & when to die are we really choosing what the patient would want or only what we can stomach. We are not the suffering one except emotionally. Right now my father is going though hell & I cannot get hospice involved no matter how hard I try to save him from this horrible existence. I am the POA and have ordered these hospice evals and he has been declined. I am quite sure he needs their help. Can’t save him the agony & no pain meds have been introduced. I know what he wants. Get get it.
As a family we are concerned about this very thing. My father recently had a filter put in his superior vena cava as he has blood clots in his legs and this will prevent a clot entering his heart, lungs and brain and killing him. He has refused to walk for three months after a two months hospital and physical rehab stay, now refusing to even sit on the side of the bed. He hasn’t wanted to walk even when he could. He has a few physical issues, phlebitis, heart, over weight, but mostly he has given up living. He has not been clear minded since this hospitalization which began 20 days ago. My brother says we shouldn’t have had the filter put in. It did feel like it would be euthanasia if we hadn’t done this as recommended by the doctors. Where are the lines?
To Kathleen – I feel so bad for you that Hospice has not been a viable option for you and your family. Is there only one Hospice in your area?
To Charlotte – As a nurse for my entire adult life, working for Hospice for the last six years, I have a simple way to show the difference between euthanasia and deferring medical treatment. In cases of euthanasia another person assists in the activity that ultimately ends life. In the case of declining medical treatment you are allowing a natural event to occur that may end up in loss of life.