by Kim Keller
I never fully appreciated how important drinking water was until my dad needed to be hospitalized — twice! — as a result of severe dehydration. He first complained about feeling extremely tired, and then he suddenly became completely confused, seemingly out of the blue. It scared us! Dad was so weak and disoriented that we needed to call an ambulance to get him safely to the hospital.
And as it turned out, the fuss was all about water.
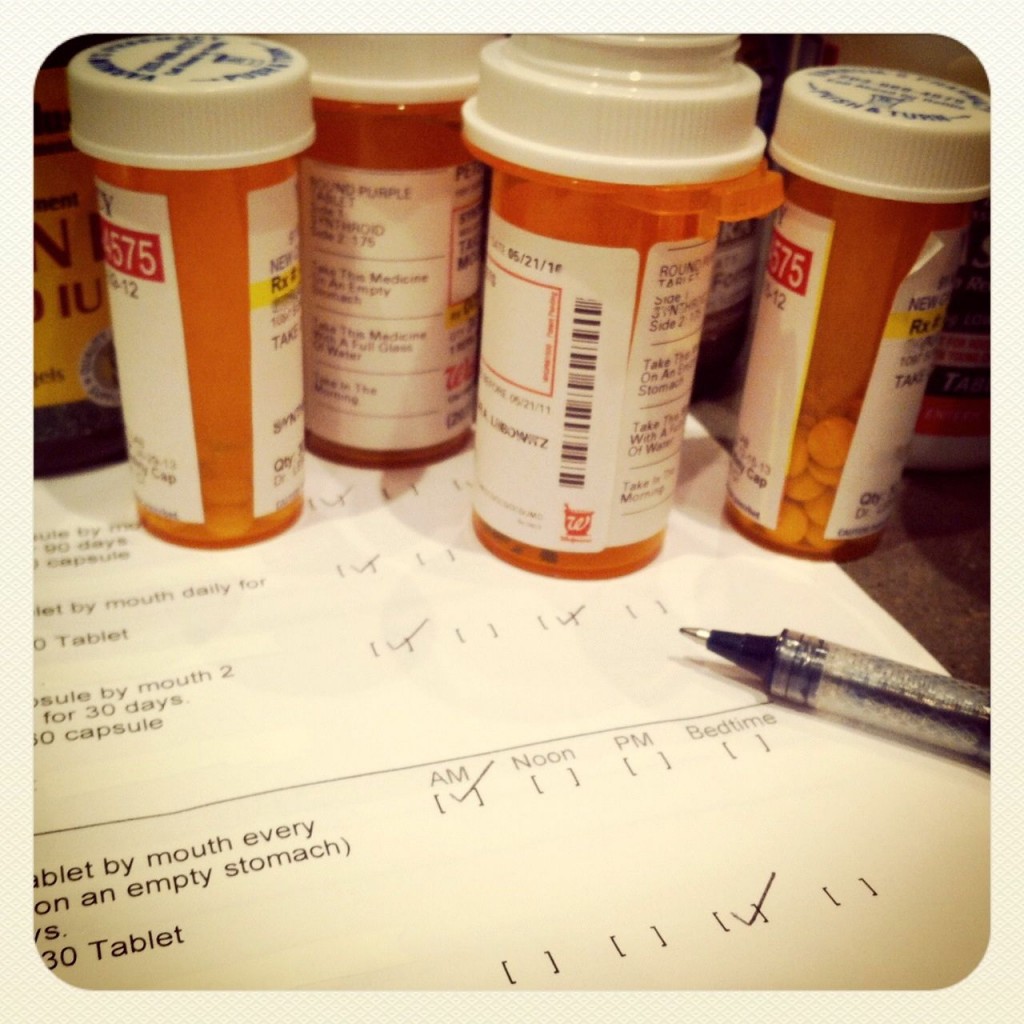
It seems so simple. Water. Yet, severe dehydration is a serious health concern for aging adults. Medications can be dehydrating. The ability to signal thirst doesn’t work quite as well anymore. The ability to store fluids diminishes. Those with dementia can no longer keep track of their water intake. And, for many, the dismay of incontinence makes all fluid intake extremely undesirable.
My sister Karen and I became relentless reminders with our dad, and now with our mom, to drink more water! Talking with friends, we’ve discovered that we aren’t alone. Many of them have experience with this issue as well.
So we asked for some of their tips, and here’s what they told us:
“I am always trying to get my mom to drink more water. Part of the problem is not knowing how much she drank. I always suggest that she put water in a quart bottle and I tell her she needs 2 bottles a day. That way she always knows how much she had.”
~ Mindy, art restorer, Weston, CT
“Most older adults, I have found, if they drink water at all, handle it better in small doses — meaning a small glass, but fairly consistently throughout the day. Encourage drinking a full (small) glass when taking meds, which is usually at least twice daily. I encourage clients to drink about half the small glass before taking the meds, so they go down easier. I try to get them to also drink a full glass (even if it’s small) with every meal. Make it a routine.
“I think water can be boring and uninteresting for many older adults, so we put it “on the rocks,” or we add a splash of OJ, grapefruit juice, cranberry, etc., to mix things up. (Be sure to check if there are any issues with medication interactions here.) We’ve even added a maraschino cherry for fun.”
~ Kathy, a gerontologist and eldercare manager, Hartford, CT
“I recently bought something called a citrus zinger water bottle. It has a juicer on the bottom for lemons, limes and oranges but can also be used for fruit of all kinds. It flavors the water, which sometimes is what’s missing for people: raspberries and lime, blackberries and lemon, melon and mint, etc.”
~ Karla, Darien, CT
“What is their favorite drink? Coffee? Then put liquids in their favorite coffee cup and make sure it’s hot. Whiskey? Then pour apple juice in a favorite whiskey bottle and warm it up in the microwave. Juice? Then pour water in a red-pebbled glass so that it looks like juice. Martini? Pour water in a martini glass and add olives. When it looks like their favorite drink, they are more likely to drink it.”
~ Jolene Brackey, author of Creating Moments of Joy for the Person with Alzheimer’s or Dementia.
“In the last couple of years of my father’s life, he would get so dehydrated that he’d have these episodes. He’d lose contact with reality, start calling out, and become incoherent or delusional. It was always a big emergency, involving ambulances and rushed visits to the hospital. One time they almost had to turn a plane around on the way to Florida. We did everything we could think of to entice him to drink. There was always a water bottle, fruit juice, his favorite drinks like Cel-Ray soda (we had to get it from NYC; soda that actually tastes like celery), non-alcoholic beer or soup at hand. It seemed like we asked him to take a sip of water at the beginning of every other sentence.
“The only time he requested water was one time that he came out of a coma. He was “nothing by mouth” at the time. He asked me for water, and it was quite the moment because we had been told he was not going to wake up, that he was going to die that night. So I had to refuse him. His eyes flew open. He thought it was so funny after all the times that I had asked him to take a drink. He said, ‘WHY? WHY??’ and then asked for the nurse. When she came, he said, ‘Tell her what you just told me.’ I repeated my refusal about the water. The nurse confirmed the medical orders and then went and called his doctor at 1 a.m. to have the orders reversed. When she came back in, she asked him what he wanted. ‘I want what I can’t have,’ he said, meaning Scotch. But he finally agreed to some water.
“I tell this story because I would have to say that, while we were very committed and resourceful in taking care of my dad, I always felt embarrassed when he had these episodes, as if I hadn’t been taking good enough care of him, as if it should have been so easy to simply give him water. So that would be my first piece of advice: to hope that people won’t feel embarrassed when this happens. The other things we learned to look for was his skin tenting or his tongue being wrinkled, but we really could have used a better way to anticipate these episodes.
“It would have been better if we could have made an arrangement to bring him in for an IV drip or, better yet, to have it available at the house, rather than wait until we had to call an ambulance because, by that point, it was very difficult to move my dad around. There were many times, taking care of Dad, that I felt like simple remedies were not available to us. These things would have made our lives easier at such a difficult time, but there was no place for simple solutions in a system that had a rule and a procedure for everything.”
~Grace, photographer, Block Island, RI
Continue Reading